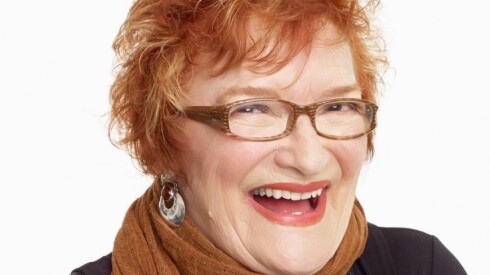
Chantal Panozzo and her husband followed their primary care doctors’ orders last year after they both turned 45, which is now the recommended age to start screening for colorectal cancer. The La Grange couple scheduled their first routine colonoscopies a few months apart.
Panozzo said she was excited to get a colonoscopy, of all things because it meant free care. The couple run a business out of their home and pay more than $1,400 a month for their family of four for coverage under the federal Affordable Care Act.
By law, preventive services — including routine colonoscopies — are available at zero cost to patients.
“This was our chance to get our free preventative care,” Panozzo said.
Their results came back normal, she said.
Then, the bills came.
The patients: Chantal Panozzo, who uses her maiden name professionally, now 46, and Brian Opyd, 45, are covered by Blue Cross and Blue Shield of Illinois.
Medical services: Two routine colonoscopies.
Service provider: Illinois Gastroenterology Group in Hinsdale. The practice is part of the private equity-backed GI Alliance, which has more than 800 gastroenterologists in 15 states.
Total bill: For each colonoscopy, the practice charged $2,034 before any insurance discounts or reductions. After discounts, Blue Cross and Blue Shield of Illinois said it was responsible for paying $395 for Opyd’s screening and $389 for Panozzo’s.
Yet, apart from the screening costs, the total included a $600 charge for each patient — though insurance documents didn’t say what that was for. This left Panozzo and Opyd each with a $250 bill — the amount allowed by BCBS of Illinois, which was applied to their deductibles.
What gives?: The couple’s experience exposes a loophole in a law that’s intended to guarantee zero-cost preventive services: Health care providers are allowed to bill however they choose as long as they abide by their contracts with insurers — including for whatever goods or services they choose to list and in ways that could leave patients with unexpected bills for “free” care.
After their screenings, Panozzo said she and her husband each saw the same unexpected $600 charge from the Illinois Gastroenterology Group on their insurance explanation-of-benefits statements. Bills from the gastroenterology group said these charges were for “surgical supplies.” Her insurer eventually told her the codes were for “surgical trays.”
At first, Panozzo was confused. Why were they receiving any bills at all?
The Affordable Care Act requires preventive care services — procedures such as colonoscopies, mammograms and cervical cancer checks — to be fully covered, without any cost to patients.
Policymakers included this hallmark protection because cost can deter many people from seeking care. A 2022 KFF poll found that roughly four in 10 adults skipped or postponed needed care due to cost concerns.
Under the law, though, it’s the insurer’s responsibility to make preventive care available at zero cost to patients.
Providers can exploit this loophole, according to Sabrina Corlette, a research professor and co-director of the Center on Health Insurance Reforms at Georgetown University.
“The insurance company is supposed to pay the full claim, but there is no requirement on the provider to code the claim correctly,” Corlette said.
In the suburban couple’s case, BCBS of Illinois covered the full cost of the screenings, according to its documents. But those documents also show that each patient was left on the hook for a portion of their separate $600 charges.
Panozzo thought a call with the insurer would quickly fix the mistake. But she said she spent most of her time on hold and couldn’t get an answer about why the colonoscopy came with a separate charge for supplies.
BCBS of Illinois declined to comment despite receiving a waiver authorizing the insurer to discuss the case.
Panozzo said a billing representative at the gastroenterology practice told her the extra charge was part of an arrangement the practice has with BCBS. She recalled being told that the practice was accustomed to keying in a billing code for “surgical trays” in lieu of a separate fee, which was described to Panozzo as a “use cost” for the doctor’s office.
“I was getting a different story from any person I talked to,” Panozzo said.
Each side was telling her the other was responsible for removing the charge, she said.
The resolution: Panozzo contested the $500 she and her husband owed by filing appeals with her insurer, lodging a complaint with the Illinois Department of Insurance and writing to her elected officials that Illinois consumers were being “taken advantage of” and “ripped off.”
Ultimately, BCBS approved both appeals, saying neither Panozzo nor her husband was expected to pay the charges.
An administrative employee at the Illinois Gastroenterology Group location where the couple was treated would not comment and directed a reporter to contact an executive with GI Alliance, the national group that manages the practice. Neither the executive nor media relations representatives responded to requests for comment.
Panozzo said that, in the past, she would have just paid the bill to avoid wasting time haggling with the doctor and insurer. But getting hit with the same bill twice was too much, she said.
“If change is ever going to happen, I need to stop accepting some of these bills that I knew were potentially incorrect,” Panozzo said.
The takeaway: Medical providers have broad leeway to determine how they bill, even for preventive services. This means patients can end up stuck with charges for unfamiliar or even bizarre things.
Research has found that private equity ownership, which has been increasing in specialties like gastroenterology, can lead to higher costs for patients as well as lower quality care.
For patients, “Under federal law, there is no recourse,” Corlette said.
State regulatory bodies may go after these providers for billing patients for covered services, but that can be a mixed bag, she said.
Insurers should crack down on this kind of practice with the providers participating in their networks, Corlette said. Otherwise, patients are stuck in the middle, left to contest what should be free care — and at the mercy of the insurance appeals process.
SEE THE BILLS
KFF Health News is a national newsroom that produces in-depth journalism on health issues.